As a leading acupuncture and integrative medicine practice, we are dedicated to supporting women in their later reproductive years. Perimenopause, the years leading up to the final period, and menopause, defined after 12 consecutive months without a period, are challenging times of significant change in a woman’s life, often fraught with challenges and uncertainty. Unfortunately, most women do not feel informed or prepared. According to estimates, while around 80% of women experience menopausal symptoms, only 19% of women ages 40-60 receive a diagnosis of menopause, let alone perimenopause, an indication that it is very common for women to navigate these transitions without guidance.
Our experienced team is dedicated to equipping women with the knowledge and resources needed to confidently navigate these stages with personalized, integrative treatment plans that blend conventional and integrative medicine approaches in order to restore hormonal regulation and alleviate common symptoms.
This article goes over the changes women experience during perimenopause and menopause and demonstrates how a personalized, integrative approach can effectively manage these changes, alleviate symptoms, and enhance overall health and quality of life. For the purposes of this article, we focus on menopause that occurs naturally and the preceding years, as opposed to surgically- or chemotherapy-induced menopause.
A Woman’s Hormonal Symphony
Estrogen and progesterone are the two main players that we’ll focus on here. Estrogen is often dubbed the ‘queen’ hormone because of its vast responsibilities. Estrogen has over 300 tasks in the body, according to Sarah Gottfried, MD1. Some of its primary jobs are:
- Maturing an egg to ovulate every month
- Building up the the uterine lining for potential pregnancy
- Helping brain function for cognition and good mood
- Contributing to maintaining good muscle mass
- Contributing to to healthy blood sugar balance
- Lubricating joints and skin
- Assisting in good libido
Progesterone can be thought of as estrogen’s calmer sister. Some of her main jobs include:
- Moderating estrogen’s effect on the uterine lining to temper bleeding
- Promoting a positive calming effect on the brain
- Promoting good sleep
- Thought to play a role in reducing inflammation and moderating the immune system
A woman’s estrogen and progesterone levels peak between her 20s and early 30s. These hormones, along with the brain and endocrine system, form a harmonious hormone orchestra governing the menstrual cycle, ensuring regularity and minimal PMS symptoms, with ideally little to no pain.
Perimenopause: A Slow March of Change
Commencing in the mid-to-late 40s, perimenopause symptoms signal the slow, gradual change in a woman’s hormones leading up to menopause. Perimenopause lasts an average of four to seven years, possibly up to ten. Ovarian function shifts gradually over time, guided by brain hormones, until the ovaries finally ‘retire’ at menopause. At first, the hormone shifts are so subtle one may not notice.
The experience of perimenopause varies greatly among women. Some continue to have regular periods and minimal hormonal symptoms throughout their 40s until menstruation gradually stops. Others are much more sensitive to hormonal dysregulation, and experience heightened symptoms starting as early as the late 30s.

What are the First Signs of Perimenopause?
A big clue to early perimenopausal changes is that menstrual cycles decrease in length. A woman who had 28-day cycles like clockwork will notice the total cycle length shortening to 26 or 25 days. She may also have a lighter flow in early perimenopause, but the biggest sign is a shorter total cycle length. This change is due to a decrease in progesterone production.
Estrogen also plays a significant role. The ovaries are winding down their production of eggs, but still receive bursts of hormones from the brain that stimulate high estrogen in the body’s attempt to ovulate. Since these bursts are erratic and not on a predictable schedule, it can cause high estrogen one cycle and low production the next.
Common Perimenopause Symptoms
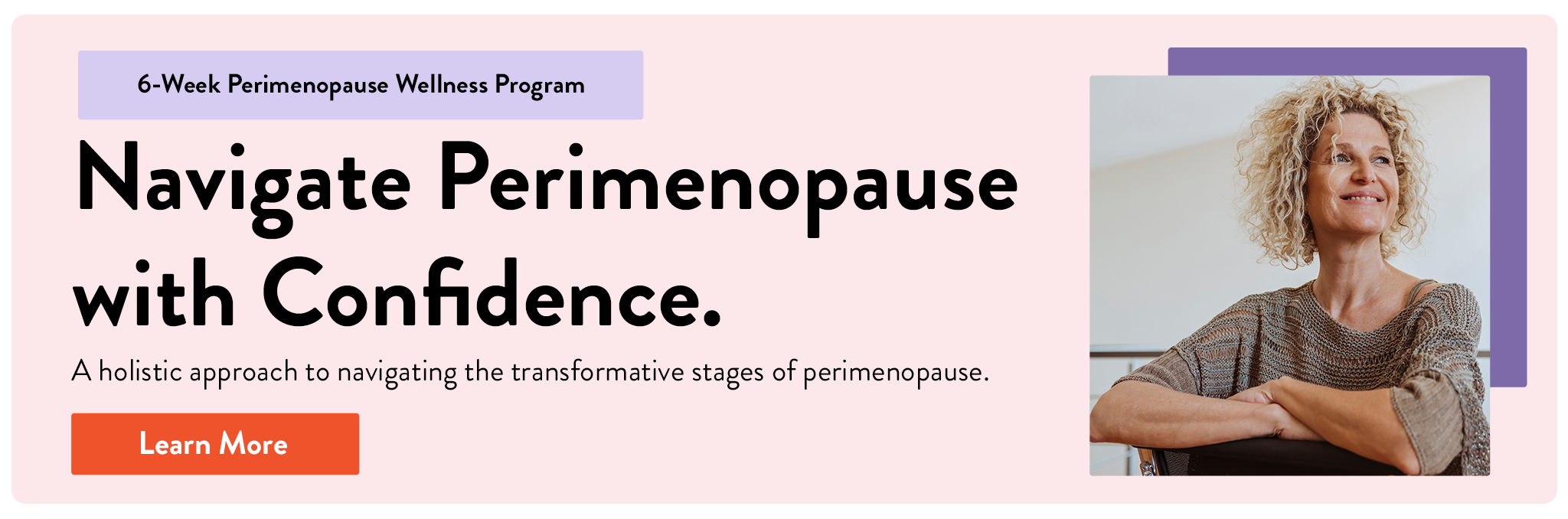
In addition to a shorter cycle, low progesterone symptoms may include:
- Increased PMS and mood changes
- Anxiety–remember progesterone has a soothing effect on the brain, so as that calming sister plays hooky, worry tends to increase
- Sleep disruptions–lighter, restless sleep in the 3-7 days before the period starts–again a result of that AWOL calm progesterone
- Weight gain–especially around the middle. Remember Queen Estrogen? Without her constant presence, metabolism can become less forgiving with the same foods and drinks that were previously handled well
- Fatigue
- Depression
- Irregular bleeding. Dr. Jen Gunter, author of the Menopause Manifesto2 calls this ‘menstrual mayhem’. Remember, estrogen thickens the endometrial lining and coordinates with progesterone to stabilize the lining. As estrogen production jumps from high to low, it can destabilize the uterine lining. The result is heavier or erratic bleeding
Understanding Menopause
Menopause is only defined retroactively, when there has been no period or bleeding for one year. The average age of menopause in the industrialized world is 513 (meaning on average women stop cycling altogether at age 50). Progesterone decreases through the 40s in a relatively predictable downward trend. Estrogen, however, fluctuates greatly in perimenopausal years, low in one cycle and surging during the next one. Estrogen finally stabilizes into a low set point closer to the end of reproductive life, in the year or two before the final menstrual period when the ovaries are really close to retirement.
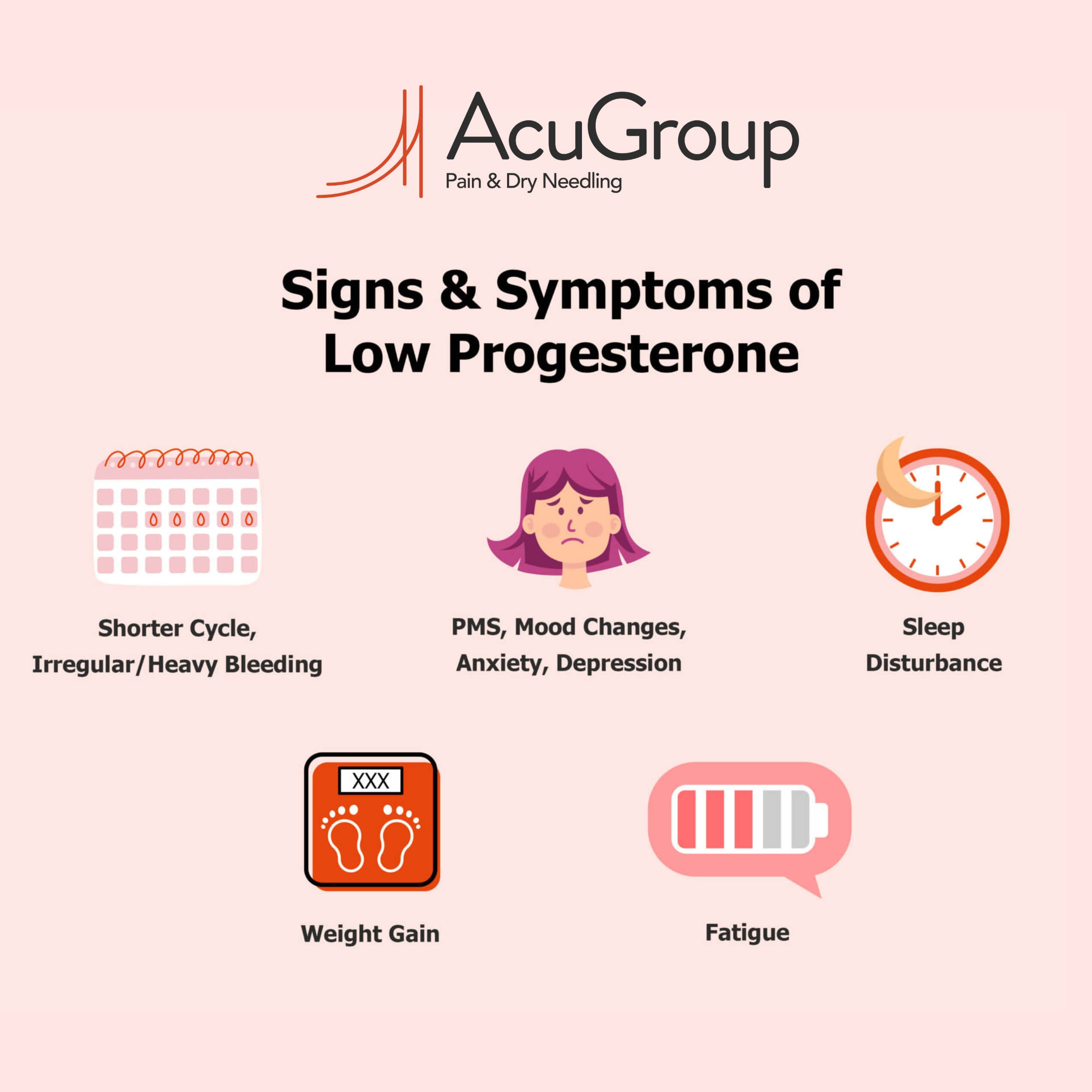
Signs and symptoms of low estrogen may include:
- Hot flashes
- Night sweats
- Vaginal dryness
- More frequent UTIs or urovaginal irritation
- Poor memory
- Mood swings
- Weight gain
- Reduced sex drive
The Impact of Stress on Hormones
“Tired and wired.” So many women identify with this experience–feeling fatigued and draggy throughout the day, but maddeningly unable to rest deeply at night. This is most often a reflection of ongoing stress. One of our stress hormones, cortisol, becomes dysregulated with chronic stress and causes problems both with sleep and daytime energy. The problem in perimenopause is that these ongoing pressures take a worse toll when our estrogen and progesterone are decreasing. High stress and cortisol almost always exacerbate hormonal symptoms1. (In fact, hot flashes experienced far before the end of menses are often a sign of high cortisol rather than low estrogen.)
Why do issues of stress take center stage in perimenopause? Consider that by their mid-to-late 40s, many women have been juggling multiple roles for a decade or more–perhaps raising kids or teenagers, planning for college tuition(s), maturing in work roles, and or taking on greater caretaking roles for older family members. These life circumstances collide with hormone depletion right at the moment when reserves have been overtaxed for years.
Organ reserve is the ability of an organ to function beyond its baseline needs. In the perimenopause years the adrenal glands take over many of the jobs that the ovaries previously performed, like a key employee going into retirement and her co-workers taking on tasks that she previously performed.
An important goal of an integrative approach to perimenopause is to help women rebuild their reserves (especially adrenal reserves) that have been depleted over years of too many demands.

Managing Perimenopause and Menopause–Moving Into Your Second Spring
This all sounds very challenging. However, it is possible to support hormonal regulation and improve the experience of hormone transition before menopause through preventive measures. And let’s not forget the wonderful benefits that can accompany the end of reproductive cycles. As a woman stops cycling for good, she’ll no longer be on a continuous cycle of up and down hormone phases. Some women’s health experts refer to this phase as a ‘second spring’. Our brain chemistry is no longer subject to highs and lows of changing hormones, nor hormones that prime us to care for others. As a colleague of mine likes to say, it’s like plugging into direct current rather than alternating current! With one steady set point, women can experience a new emotional freedom and confidence to pursue life goals and desires.
Hormone Replacement Therapy (HRT)
Estrogen receptors are widespread, present on cells throughout the body. As such, the diminishing levels of estrogen that occur during perimenopause and menopause can significantly impact daily life. One solution to manage these changes is hormone replacement therapy (HRT), which supplements estrogen, and in some cases progesterone, offering significant improvements to perimenopausal symptoms for numerous women.
HRT does come with risks and potential side effects, which unfortunately have been blown out of proportion due to years of negative media representation and misinformation. This largely stems from a misinterpretation of the results from The Women’s Health Initiative, the largest study on HRT. The primary issue was the focus on an older demographic than the typical hormone therapy recipient, which has since led to many potential beneficiaries shying away from this treatment. For a comprehensive review of this history, we recommend the New York Times Magazine piece “Women Have Been Misled About Menopause,” or the book “Estrogen Matters” by Drs. Avrum Bluming and Carol Tavris4.
The North American Menopause Society, the American Society for Reproductive Medicine, and The Endocrine Society, leading women’s health and menopause, have issued a joint statement asserting, “Most healthy, recently menopausal women can use hormone therapy for relief of their symptoms of hot flashes and vaginal dryness if they so choose.”
However, it is important to be cognizant of the potential risks associated with supplemental hormones. For women with an intact uterus, both estrogen and progesterone need to be taken, while those who have had a hysterectomy only require estrogen. As per the joint statement, “Both estrogen therapy and estrogen with progestogen therapy increase the risk of blood clots in the legs and lungs, akin to birth control pills, patches, and rings. While these risks are rare in the 50 to 59 age group, they do exist. Moreover, continuous use of estrogen/progestogen therapy for five or more years may slightly elevate the risk of breast cancer. However, the risk decreases after discontinuation of hormone therapy.”
It is essential that these risks are thoroughly evaluated in consultation with an OB/GYN or a qualified healthcare provider, taking into account both your family history and personal medical history.
Personalized Perimenopause and Menopause Treatment: An Integrative Approach
Navigating perimenopause and menopause doesn’t have to be a solitary journey. Our integrative treatment approach combines natural and pharmaceutical therapies for a balanced physical, mental, and emotional well-being. Recognizing that each patient is unique, we offer personalized programs based on your health history, goals, and preferences. For women navigating hormonal changes, this tailored approach entails:
- Identifying where you are in your perimenopause to menopause journey:
- By tracking your menstrual cycle length and ovulation patterns, and running hormone tests where necessary, we can better understand your individual hormonal profile.
- Assessing the root causes of your symptoms:
- We delve into your health history to identify and address possible contributing factors to your current symptoms.
- Incorporating a holistic view of your health:
- We understand that hormone regulation affects multiple body systems. For instance, with the decline of progesterone and erratic estrogen levels, the adrenal glands become more actively involved in hormone modulation. We support these connections through comprehensive health strategies such as stress management and digestive health support.
- Addressing stress:
- We help you discover personal stress relief methods crucial for rejuvenating your vitality.
- Personalizing treatment:
- Whether your metabolism remains unchanged or you’re grappling with energy and blood sugar imbalances, we provide tailored solutions to meet your specific needs.
- Utilizing specialty testing:
- To understand your hormone, adrenal, and gut status better, we use specialized tests.
- Collaborating with other healthcare providers:
- To ensure you have access to all necessary tools, we partner with physicians and specialists who can offer complementary treatments
Integrative Tools for Hormonal Regulation
Acupuncture
- Acupuncture stimulates the relaxation response in your nervous system, helping to regulate stress hormones like cortisol. Each treatment is relaxing, and it also helps downregulate the fight-or-flight response over time.
- Acupuncture demonstrates substantial benefit for various hormonal symptoms, including hot flashes and night sweats. In a 2016 randomized control trial, researchers at Duke University studied the effects of acupuncture on hot flashes in 209 women. One-hundred-seventy women received 20 acupuncture treatments, at a frequency of just over once a week. After only three to four weeks, symptoms improved. By eight weeks of treatment, participants reported 34% reduction in frequency of hot flashes. Twelve percent reported an 85% drop. In 2018, a meta-analysis of seven studies also concluded that acupuncture effectively reduces menopausal hot flashes.
Nutrition
Nutrition is a great opportunity to feel your best and contribute to a ‘new normal’ of vitality in midlife. Here are some examples of nutrition guidance:
- Eating a nutrient dense diet–focus on fresh, simple foods as a main power source along with lean proteins. Fill up on nature’s best! A lower carbohydrate diet rich in a wide spectrum of veggies is the right choice if blood sugar levels are high. The Mediterranean diet has demonstrated excellent results for weight management and reduction of hormone symptoms for perimenopausal and menopausal women.
- Changing metabolism means using different fuels. Revise your diet to limit sugar, alcohol and refined grains. They offer few to no nutrients, destabilize the blood sugar and mood, and drive inflammation.
- Meal timing–people are generally more insulin resistant as the day goes on. That means that the body uses calories more efficiently in the morning. The same number of calories at night when our body slows down for sleep can result in more weight gain over time.
Supplements and Herbs
Natural substances, including adaptogenic herbs and specific Chinese medicine blends, can be a huge help to modulate the body’s hormones and stress responses.
- For example, a commonly prescribed Chinese herbal formula, Er Xian Tang, was evaluated in a randomized controlled trial. The blend was given to 101 women for menopause symptoms for 3 months. The formula reduced hot flash frequency by over 50%, reduced total hot flash scores, and the treatment group showed greater increases on the Menopause-Specific Quality of Life score than placebo group.
- Maca (Lepidium peruvianum) shows great effect on the master hormones in the brain that govern not only estrogen and progesterone, but also thyroid function. Because it’s thought to work more on the level of the brain, maca is a wonderful balancing plant for many women.
Lifestyle
Essential activities like regular movement and exercise, restorative practices and making time for pursuits that foster joy and connection. For example:
- Intensity and frequency of exercise–As much as we need movement, intense cardio may not be the right recipe for midlife women because it can raise cortisol levels. Exercise programs that focus on fun, and strength-building exercise are often better for metabolism and well-being.
- Yoga or gentle mind-body practices–This type of movement offers benefits to hormones, with studies showing that yoga reduces intensity and severity of hot flashes.
- Spending time with female friends is hormonally beneficial for many women. This is known as the ‘tend and befriend response’. Women get lower stress and infusions of oxytocin (the ‘love hormone’) when we regularly laugh, commiserate and commune with our female friends. Exercise with a friend for a double win!
Get Personalized Guidance
Remember, you don’t have to navigate these life transitions alone. If you’re embarking on a journey towards hormonal support, our expert team is here to guide you and help you thrive through perimenopause, menopause, and beyond.

Notes
1. Gottfried, Sara. The Hormone Cure: Reclaim Balance, Sleep, Sex Drive, and Vitality Naturally with the Gottfried Protocol. Simon & Schuster, 2014.
2. Gunter, Jen. The Menopause Manifesto: Own Your Health with Facts and Feminism. London: Piatkus, 2021.
3. Berry, Katherine. Menopause: A Comprehensive Guide for Practitioners. S.l.: EASTLAND PR, 2023.
4. Bluming, Avrum, and Carol Tavris. Estrogen Matters: Why Taking Hormones in Menopause Can Improve Women’s Well-Being and Lengthen Their Lives– without Raising the Risk of Breast Cancer. First edition. New York: Little, Brown Spark, 2018.
5. Breiden, Lara. The Hormone Repair Manual: Every Woman’s Guide to Healthy Hormones After 40. Greenpeak Publishing, 2021
Medical Disclaimer
The information provided in this article is intended for general informational purposes only. It should not be considered a substitute for professional medical advice, diagnosis, or treatment. Always consult with your healthcare provider before starting any new treatment or health program.